Many forms of cancer have been treated using systemic radiotherapeutics, which can destroy cancer cells, their ability to replicate or both.
However, these drugs may also attack other, healthy tissues on their way to the target tumour, which results in severe side-effects for the patient and explains why radiotherapy can have such a profound negative effect on the body during a course of this treatment. Therefore, medical scientists and researchers have been working for some time to develop these therapies so that they attack cancer cells with much more accuracy and specificity.
Potential new forms of therapy
This has also led to alternative treatment types such as phototherapy and photodynamic therapy, in which light is introduced directly at or into a tumour in order to induce death and ‘pro-death’ biochemical processes in such a mass.
A new study introduces a modified combination of specific chemotherapy and phototherapy, which also incorporates PET (a form of medical imaging) to activate this new treatment. This comprehensive form of therapy could combine diagnostic imaging and treatment in the cancer clinic of the future.
Cancer can be detected and tracked in the clinic through the use of non-invasive imaging techniques. They can show the tumour as 2D or 3D images on computer screens that help an oncologist to assess the severity or progression of a patient’s condition.
Some of these techniques are based on radiation or particle types that pass through the body and are captured for image creation determined by the differential densities of different tissues (cancers included), which changes the amount of this energy that gets ‘through’ them. Others, however, pick up signals from radioactive or fluorescent ‘marker’ molecules that are readily taken up by the tissues or masses of interest, thus giving very clear and accurate pictures of where they are in the body.
An example of fluoromarker-enhanced imaging is positronic-emission tomography (PET), which offers imaging based on the uptake of fluoro-deoxyglucose (FDG). FDG is a modified form of the body’s most efficient energy source, which is also rapidly consumed by tumours.
When a tumour takes up FDG, it ‘lights up’ under PET, as the imaging induces the fluorescent molecules attached to the glucose to ‘activate’ in vivo. This allows for accurate and specific tumour imaging. It also allows for long-term imaging in cancer patients, as it is relatively safe and highly reliable.
Therefore, PET is used to assess tumour mass and shape, and how these change in response to therapy over time. This treatment may involve radiotherapy. Archaic as this sounds, modern radiopharmaceuticals can target cancer cells specifically, invade them and release a very localised burst of radiation. This can lead to a variety of destructive and eventually fatal effects within the cell.
An example of this ‘close-quarter’ radiotherapy is a molecular vehicle that releases a tiny amount of radioactive matter. They require the donation of electrons or positrons, usually from a metal (which can also be incorporated into the radionuclide in nanoscopic form) to release specific radiation types.
These include Cerenkov radiation, which is the emission of light in the ultraviolet-to-blue range by beta-radiation particles. This results in the generation of reactive oxygen species (ROS) in the immediate vicinity. ROS is toxic to cancer cells (and normal cells) and can induce cell death in a variety of ways. This technique is known as Cerenkov radiation-induced therapy, or CRIT. CRIT radionuclides can be delivered through their packaging into nanostructures that target cancer cells by detecting and binding to cell-surface proteins that are particular to cancer cells. These structures then introduce the radionuclides into cells by passing through or otherwise interacting with cellular membranes.
However, it would also be best if this chemo-radiation reaction could be predicted and controlled by oncology professionals, so as to limit the risks that CRIT could also affect healthy tissues surrounding a tumour. Therefore, a team of researchers, led by Professor Samuel Achilefu from the Washington University School of Medicine’s departments of radiology and medicine, set out to develop a new therapy that combined radionuclides, nanostructures to deliver them and PET to activate them.
This was done using a type of radiopharmaceutical called titanocene that could release Cerenkov radiation in response to the light released by FDG. Therefore, this therapy would also be controlled using PET. The nanostructures were tiny micelles, which are made of molecules that are similar enough to cell membranes to be able to integrate into them in order to release their contents. The nano-micelles were also engineered to bind VLA-4, which is expressed on the surfaces of some cancer cells, including melanoma cells. The team tested their new therapy on experimental melanomas developed in mice.
By Jens Maus (http://jens-maus.de/) - Own work, Public Domain, Link
The researchers found that the titanocene-containing micelles were taken up readily when introduced into mice with tumours, and that they were present in large amounts in areas likely to be invaded by melanoma cells. They then added conventional medical-grade FDG to the active treatment, and confirmed that both this compound and the nano-micelles were accumulating in tissues also infiltrated with melanoma. Mice with melanoma treated with both FDG and nano-micelles, then imaging using PET, exhibited a progressive decline in disease progression, whereas control mice treated with either FDG or nano-micelles experienced an exponential increase in cancer-cell counts over time.
The survival rates in the mice receiving the ‘complete’ treatment were also significantly greater compared to those in the control group. However, the team also found that the active treatment did not kill a small sub-population of the melanoma cells, due to a low level of a protein called CD49d (or alpha-4) that is required to activate VLA-4. Therefore, these cells were inadvertently resistant to nano-micelle binding.
Accordingly, the team took a different approach to the vehicle for titanocene delivery, namely human serum albumin (HSA). HSA nanostructures were found to be able to hold a high concentration of radionuclide, and could also distribute itself well into tissues typically affected by tumours in a mouse model of breast cancer. However, this did not address the sparing of healthy tissues, and was also susceptible to resistance in a small subgroup of cancer cells.
However, the treatment did spare the stem cells found in bone marrow. Radio-chemotherapy can destroy these cells in the normal course of treatment, which is a prominent concern for doctors and patients who need to manage this long-term adverse effect.
This treatment may not be the super-effective ‘imaging-powered nanosurgery’ procedure for tumour destruction that Achifelu and his team may have envisioned while constructing this project. On the other hand, the study demonstrated the improved efficacy of titanocene as a result of its combination with targeted nano-micelle delivery and activation with FDG-PET.
It also showed that targeted titanocene activated through its imaging resulted in significantly prolonged survival in a mouse model of melanoma. Therefore, it could be applied to similar cancers (i.e. of the type that create relatively small tumours, yet are highly metastatic) with further refinement. This development may have to involve solving the problem of resistance to the treatment, in which some cancer cells do not allow the otherwise specific CRIT vehicles to bind and invade them.
Radiopharmaceuticals are falling out of favour in modern cancer treatments due to their side-effect profile and lack of efficacy in the absence of targeted delivery. However, a new method of conveying these drugs directly into cancer cells and activating their ROS-producing radiation using FDG-PET has been documented in a recent Nature Communications paper. This technique increased the specificity and efficacy with which titanocene reduced tumour growth in mouse models of cancer.
It should be noted that the pharmacokinetics of the drug (e.g. its clearance) mandated rather precise timings for its administration relative to that of the FDG with which it is activated in vivo. In addition, scientists who want to work on this technique may need to find a surface receptor that is more common to a total population of cancer cells to be killed, or develop a completely new proposal to address the treatment resistance seen in the initial study. Presuming this can be achieved, future work on this promising ‘PET-activated radio-therapy’ may lead to a new option in the treatment of some cancers one day.
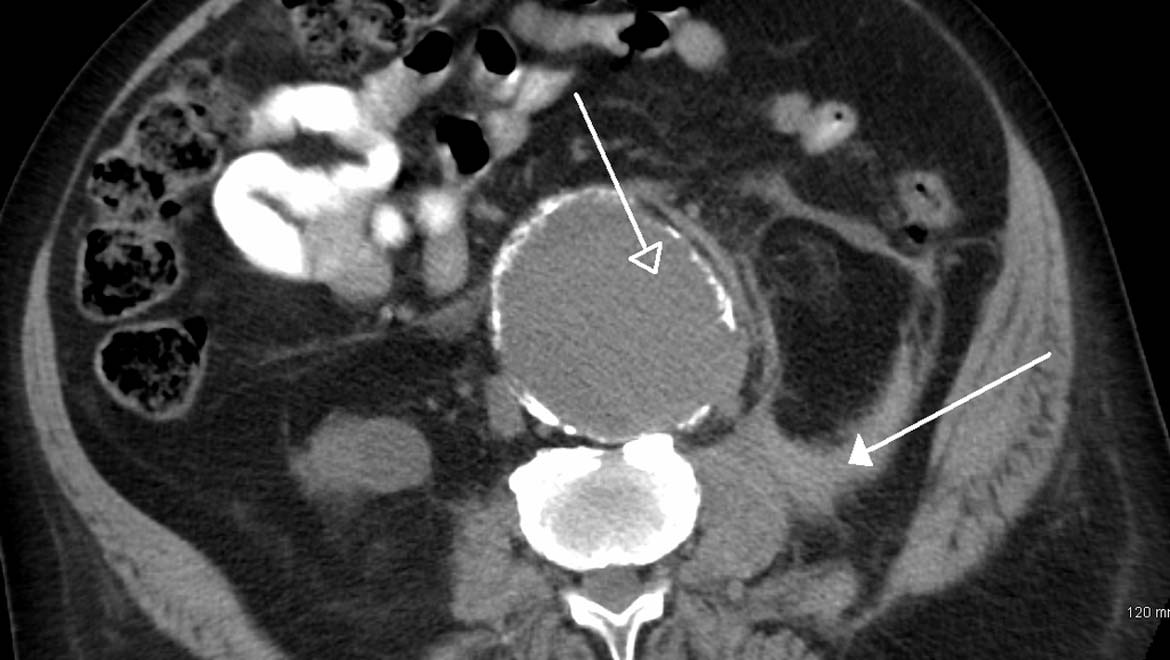
Top image: A ruptured AAA as seen on CT. (CC BY-SA 3.0)
References
Kotagiri N, Cooper ML, Rettig M, Egbulefu C, Prior J, Cui G, et al. Radionuclides transform chemotherapeutics into phototherapeutics for precise treatment of disseminated cancer. Nat Commun. 2018;9(1):275.
Shaffer TM, Pratt EC, Grimm J. Utilizing the power of Cerenkov light with nanotechnology. Nature nanotechnology. 2017;12(2):106-17.





No comment