Some conditions that affect the eyes may be related to toxic forms of the molecules that normally act to send visual signals to the brain. These molecules are retinal of the 11-cis (11-CR) and all-trans (ATR) variety. Therefore, 11-CR and ATR are technically the same compounds. However, they each take a different ‘shape’ in order to control the first steps in the transmission of light-based information to the brain.
Other forms of retinal, which may be breakdown products (or the products of chemical damage) of the same molecule, have been found to be toxic to cells. These cells may be in the retina, or elsewhere in the body.
These broken forms of retinal may be linked to accelerated cell death. This effect has been linked to several conditions, from night blindness to age-related macular degeneration.
Blue Light Damages the Eyes?
A more recent study has claimed a link between the exposure to blue light and the production of yet more toxic molecules, also related to retinal, in vitro. These results may indicate that excessive exposure to blue light may help the progression of eye damage, or even the loss of sight in serious cases.
Blue light emanates from sources that include UV light and the light from our device's screens. Therefore, these findings may have worrying implications for many people in the developed and the developing world.
On the other hand, it is still not clear if the results of this study translate directly to real-world blue light exposure. The researchers behind it noted that it took blue light sources of relatively high intensity (1 microWatt (µW)) to elicit dangerous effects, whereas the typical intensity needed to activate retinal under normal circumstances is closer to 0.2 µW. Therefore, it may take prolonged, protracted exposure to these sources to elicit the damaging effects evaluated in this study.
In addition, it is possible to set some touchscreen devices (mostly smartphones) to limit blue light progressively throughout the day.
Toxic Molecules Related to Blue Light Exposure
Traditionally, it has been thought that cytotoxicity (or increased cell death) occurred in the retina due to the production of lipofuscins. These include derivatives of retinal such as N-retinylethanolamine. Alternatively, they may be dimers or adducts (two retinal molecules or fragments that have become ‘stuck’ together, unusually) of retinal.
Lipofuscins arise when the normal metabolism of retinal (in which the same retinal molecule is converted from 11-CR to ATR and back again in a continuous loop) is somehow impaired, leading to a build-up of ATR. This may affect eye cells in two main ways: first, the continuum of retinal conversion is necessary for it to function as a light-activated receptor (or opsin) that kick-starts the transmission of visual signals through the optic nerve. Secondly, lipofuscins are cytotoxic.
Ophthalmological scientists theorize that this cytotoxicity is mediated by the production of dangerous reactive oxygen species (ROS) and through upsetting the balance of calcium atoms in the affected cells. The newer, blue-light-associated mechanism of cell death may also involve calcium cytotoxicity.
However, in this case study, it was found to involve a common cell membrane component called phosphatidylinositol 4,5 bisphosphate (PIP2). The scientists tested the theory that blue-light-exposure (BLE) altered the function of normal retinal in a way that caused the molecule to hydrolyze PIP2 and cause it to migrate into the cytosol (or internal space) of the cell. The team modified HeLa cells in culture to express PIP2, bound to a red fluorescent tracer (mCherry) so that these compounds would show up under imaging.
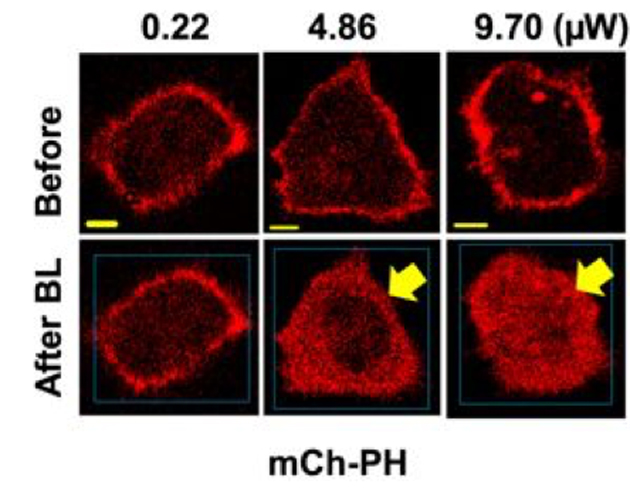
Imaging study showing the response of labelled PIP2 (mCh-PH) to ATR and BLE of increasing intensities. (Source: K. Ratnayake, et al., 2018)
The scientists found that, under BLE of 0.22µW (and at 445 nanometers), and in the presence of ATR at a concentration of 50 µM, the mCherry-PIP2 behaved normally. However, when the intensity was increased to 4.86 µW and then 9.70µW, PIP2 was observed to undergo hydrolysis and invade the cytosol. The scientists were also able to demonstrate that this property of ATR was G-protein coupled receptor (GPCR)-independent, even though normal opsin signaling is.
However, the group also observed that the hydrolysis of PIP2 was not enough to induce cytotoxicity on its own. It required the additional step of ROS production in these cells. As ROS is a possible consequence of high intensity (i.e., greater than 1 µW) light exposure, it may suggest that the potential negative effects of BLE result from extreme lighting conditions or exposure.
This study may have vindicated some concerns about the duration and extent of light exposure, particularly those that deliver blue light. As these sources include the screens that are now an essential part of our lives, it will be interesting to see if further work on this subject gives similar results in the future.
Top Image: Does blue light damage the eyes? Some researchers have found possible new reasons to think so. (Source: maxpixel.net)
References
Should You Be Worried About Blue Light? 2018, AAO, https://www.aao.org/eye-health/tips-prevention/should-you-be-worried-about-blue-light , (accessed 16 Aug. 18)
L. Zou, et al. (2015) [Blue light and eye health]. Zhonghua Yan Ke Za Zhi. 51:(1). pp.65-69.
K. Ratnayake, et al. (2018) Blue light excited retinal intercepts cellular signaling. Scientific Reports. 8:(1). pp.10207.







No comment