Type 1 diabetes is an autoimmune condition in which the patient’s ability to produce insulin is negated by their body’s own protective processes, often from an early age. As with type 2 diabetes, it can require chronic medical treatment from the point of diagnosis in order to avoid severe, even life-threatening, disease events.
This treatment may also last the patient’s entire lifetime. Therefore, many medical researchers conclude that implantable devices may be the way forward for effective type 1 diabetes treatment. A team of scientists has investigated the potential of a new and interesting implantation technique in animal models of this condition. This method may also be even capable of reversing type 1 diabetes, by replacing the affected cells in this condition.
Using cell encapsulation to treat diabetes
This technique is known as cell encapsulation. It is an innovative strategy by which cells are coated in a protective layer of a substance (often a neutral polymer) so that they will not be attacked by the immune system of an animal into which they have been implanted.
In other words, it is a possibly improved delivery system for cells (which may be in small numbers or alone) that are isolated from a donor and introduced into a new host. Cell encapsulation is seen as an exciting new option for applications such as stem-cell therapy. Alternatively, it is attracting increasing interest as a way to replace or augment the cells of pancreatic islets in those with type 1 diabetes. These cells, which produce insulin (in addition to important metabolism-related signalling molecules such as ghrelin, glucagon, and somatostatin) are attacked and destroyed by autoimmune processes in the course of this condition. Therefore, the cell encapsulation and delivery of new islet cells from a separate donor may be an effective strategy to address this form of diabetes.
The materials used for cell encapsulation have included polymers such as hydrogels, chitosan or alginate. Studies have shown that they have greatly enhanced the efficacy of donor-cell delivery to various sites and tissues; in addition, cells, once encapsulated, have exhibited viabilities of over 90%. Furthermore, stem cells released from encapsulation to grow and develop as normal have demonstrated the ability to do this as efficiently as similar, non-encapsulated cells. Therefore, encapsulation is now seen as a safe, effective delivery method for therapies that involve direct cellular replacement, which is known, somewhat aptly, as cellular therapy.
Encapsulation may be particularly amenable to type 1 diabetes, as a central goal of cellular therapy for this condition is to establish a level of islet cell density that is high enough to establish or re-establish normal pancreatic function. Therefore, an increasingly large number of studies have investigated the potential efficacy of cell encapsulation in models of the condition. In addition, encapsulation has also been used to enhance pre-existing grafting strategies for type 1 diabetes. One study demonstrated that the addition of encapsulated bilirubin (an antioxidant which may protect against cellular destruction in some settings) resulted in a significant decrease in cell death due to hypoxia within islet allografts in a mouse model of pancreatic grafting. The mice with encapsulation-enhanced grafts also exhibited a significant increase in normal glucose responses compared to those with standalone grafts.
On the other hand, these early forays into cell encapsulation for type 1 diabetes may not have some attributes that are preferable in terms of clinical applicability and development; for example, they may not be scalable. In addition, it may be better if encapsulation-based technologies could take the form of implants that could be removed when an optimal level of live islet cells has been established. This would require a capsulation polymer with appreciable mechanical strength, resilience and diffusion properties. However, some materials (e.g. alginate) may not live up to these ideals.
Developing a new method
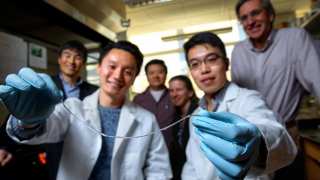
Therefore, a team of scientists collaborating across numerous institutions at Cornell; Novo Nordisk Denmark; the University of Michigan Medical School and the Chinese Academy of Sciences developed a new type of calcium-releasing nano-porous polymer with which to encapsulate rat and human islet extracts. This new material, which forms macroscopic threads, was also coated in a thin layer of alginate-based hydrogel, to which it adhered well. This complete delivery system was comparable to alginate fibres alone in terms of protecting ‘donated’ islets from the immune environment of mice with experimentally-induced diabetes. However, the new polymer’s structure was also found to be superior to standalone alginate in terms of mechanical strength and durability. It also exhibited relatively reduced diffusion, which made its mass-transfer properties more favourable for the levels of manipulation required.
The researchers were able to produce this new molecular device (which they dubbed the “TRAFFIC” islet-cell encapsulation system) in long strands, but could also cut it down to ‘fit’ the animal in question. Therefore, the TRAFFIC system may be more scalable than other systems shown in previous papers. TRAFFIC was also shown to be robust enough to be removed in full, without breakages, in laparoscopic studies in dogs. The polymer-based delivery device can be laid in long ‘chains’ leading out from the site of interest (the pancreas, in this case) towards a point at which it can be retrieved easily and safely using minimally-invasive techniques. In addition, because the materials are not immunoreactive, the chains can also lie along organs such as the liver for the duration of their implantation.
The researchers also reported that the induced diabetes of the mice used in this study was reversed as a result of implantation with rat islets delivered using their TRAFFIC system for three months. They also reported these results in mice from an immunodeficient laboratory strain that were implanted with human islets in the same manner for four months. They also scaled the system (albeit without cells) up to implantation in dogs. These animals lived with the implants for a month, after which time the chains were successfully removed in full. The team now hope that their new encapsulation system will contribute to the ultimate treatment for type 1 diabetes in humans one day.
Having type 1 diabetes often implies long-term, inconvenient and possibly expensive treatment regimens. Therefore, some patients may prefer an implantable solution, and may even opt for surgeries that may restore normal pancreatic functions. Cellular therapies may be the way forward for the treatment of those with this condition. Researchers such as those who have conducted the study as above assert that cell encapsulation is the optimal technique to deliver this treatment strategy. It is associated with impressive results in animal studies; however, time will tell if cell encapsulation is compatible with human patients.
Top image: The device created by ViaCyte contains millions of cells in packets that are implanted under the skin, in hopes they will function like pancreatic cells. THE HUMAN TRIAL / PNG
References
Fullagar B, Rao W, Gilor C, Xu F, He X, Adin CA. Nano-Encapsulation of Bilirubin in Pluronic F127-Chitosan Improves Uptake in beta Cells and Increases Islet Viability and Function after Hypoxic Stress. Cell transplantation. 2017;26(10):1703-15.
Sakai S, Liu Y, Sengoku M, Taya M. Cell-selective encapsulation in hydrogel sheaths via biospecific identification and biochemical cross-linking. Biomaterials. 2015;53:494-501.
An D, Chiu A, Flanders JA, Song W, Shou D, Lu Y-C, et al. Designing a retrievable and scalable cell encapsulation device for potential treatment of type 1 diabetes. Proceedings of the National Academy of Sciences. 2017.





No comment