Nanomedicine is a rapidly maturing sub-discipline of medicine based on the delivery of substances (mostly drugs) that are packaged into nanoparticles for delivery that may be improved, more targeted or both compared to traditional routes (e.g., metabolism following the consumption of oral formulations).
Nanoparticles may be a particularly powerful tool to shape the treatment of many neurological conditions. These disorders, which include Alzheimer’s disease (AD) or Parkinson’s (PD), may be managed effectively through molecules associated with the promotion of cellular regrowth or the reduction of dangerous reactive oxygen species (ROS) in the affected brain tissue.
Crossing the Blood-Brain Barrier
However, many compounds that may facilitate these effects fail to even reach the brain in conventional forms that must be swallowed or injected. This is because they cannot cross the blood-brain barrier (BBB). It is a complex of blood vessels, mucous membranes and other similar tissues that act as a profound divider between the central nervous system (CNS) and the rest of the human system. The BBB is an effective defence against contaminations, infections, and intoxications of many kinds.
The BBB is also complemented by the brain-to-cerebral spinal fluid barrier (BCSFB) that prevents potential, analogous spinal contaminations from reaching the brain. These two structures are indeed one of the CNS’s primary assets against damage of many kinds. However, this advantage backfires when certain people are in need of treatments that have to act at the site of degeneration in order to be effective.
Nanoparticles, however, have demonstrated efficacy in crossing the BBB and BCSFB and eliciting positive effects in AD or PF treatment studies.
This is because many nanoparticles have structures inspired by natural features such as cellular membranes. Some nanoparticles are roughly spherical in shape and are made of phospholipid molecules that interact to form ‘walls’ around a hollow core. These cores contain compounds such as drugs. The complete phospholipid nanoparticles have demonstrated the ability to cross the BBB or BCSFB and ‘unpack’ their contents much closer to the desired target in the brain.
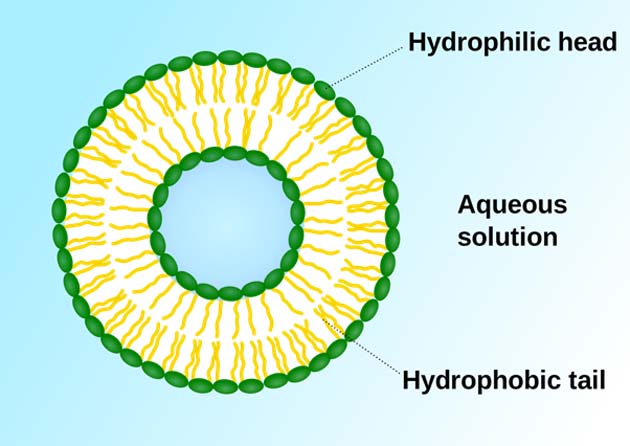
The basic structure of the liposome. (Source: Wikimedia Commons)
Drug Delivery by Nanoparticles
This type of nanoparticle, which is sometimes termed liposomes, are associated with the effective delivery of the potential PD drug glial cell line-derived neurotrophic factor (GDNF), across the BBB, which was between six and eight times greater than that of conventional GDNF formulations. Liposomes have also been used to deliver the antioxidant resveratrol and the established drug levodopa to PD-affected tissues.
However, these liposomes can still be obstructed, rejected or even destroyed by the native immune cells of the BBB/BCSFB, as they may have an ‘alien’ lipid make-up from the perspective of these cells. The BBB may block them through processes such as opsonization, in which the nanoparticles are ‘digested’ by phagocytes, which then ‘excrete’ the resulting, inert products into the systemic bloodstream, from where they are eventually passed out of the body.
However, this can be circumvented by engineering liposome surfaces that also contain more ‘host-like’ molecules. They are either more acceptable to the BBB immune system or allows the particles to be ignored by the same. The addition of chitosan or pegylated complexes has resulted in more successful liposome passage into the brain in some studies.
Restructured Nanoparticles: Lipid Liposomes
Alternatively, researchers could use another form of a nanoparticle to deliver their candidate therapy. These additional forms include lipidic particles, in which the hollow, drug-containing core is surrounded by lipids in conformations other than phospholipid walls. These include colloidal shell structures and nanoparticles made of solid lipids. These may be more compatible with the BBB immune response, and can even be stably packaged into cells in order to cross the barrier.
These type of nanoparticles have been associated with the successful delivery of GDNF and bromocriptine, which has improved on movement disorders and drug uptake by target neurons in animal models of PD.
However, non-solid lipidic nanoparticles may ultimately be the better option of the two, as they are typically associated with the ability to accommodate a greater volume of active molecules compared to their solid lipid counterparts.
Furthermore, lipid nanoparticles along these lines have shown promise in the delivery of AD treatments such as galantamine, as well as resveratrol in AD models. However, the majority of the studies showing the potential of nanoparticles in these neurodegenerative conditions have been conducted in animals or in vitro studies. Therefore, they have a long way to go before they are accepted as BBB-crossing treatments for humans.
In addition, the administration routes for these drugs are often slightly atypical compared to many drugs on the market today. They include the intragastric route, in which the nanoparticles must be injected directly into the stomach, the intraperitoneal route and the intranasal route. It is possible that they may be developed to the point that this is not necessary for human patients. However, if not, it may be a cause of discomfort or even treatment refusal in some people, particularly those already experiencing the potentially distressing effects of neurodegeneration.
In summary, nanoparticle-packaged therapies are a possible wave of the future for conditions that require negotiation with the blood-brain barrier. They may help manage the adverse effects of Alzheimer’s disease or parkinsonian conditions (e.g., motor or memory dysfunctions) based on preliminary and pre-clinical studies. However, the researchers working on these potential therapies may still have a long road ahead before the results of their studies can help human patients.
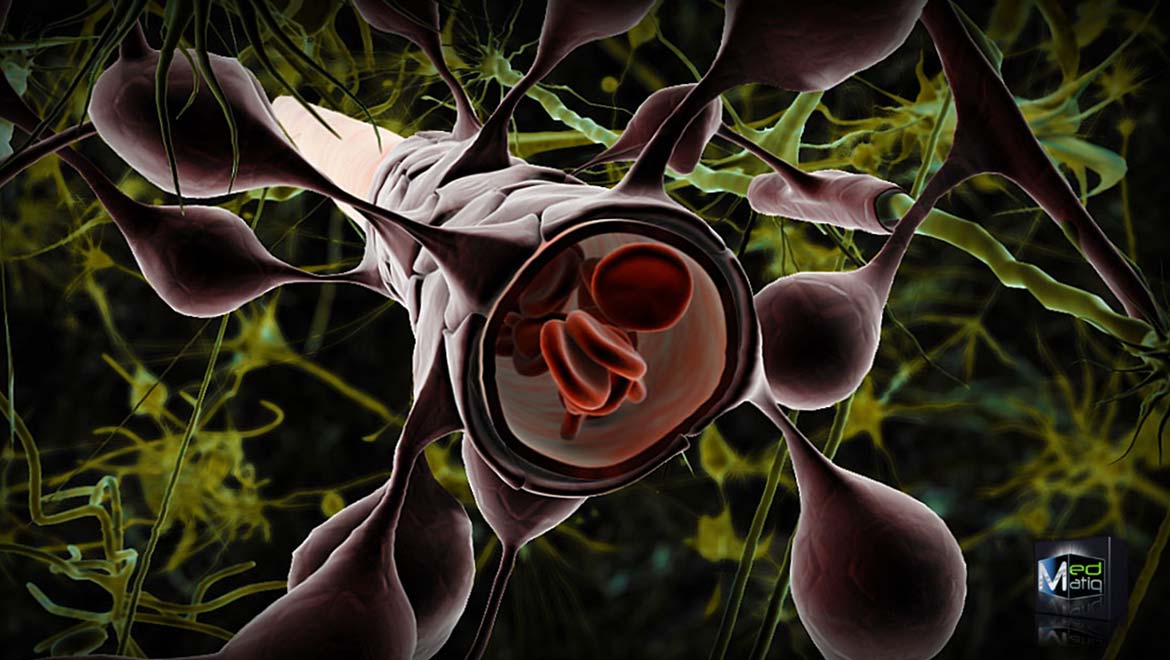
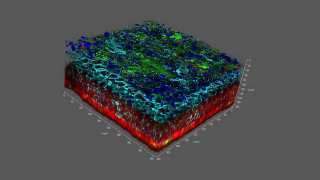
Top Image: An artistic impression of the blood-brain barrier. (Source: Ben Brahim Mohammed/Wikimedia Commons)



No comment