Diabetes is a particularly difficult condition to handle on a day-to-day basis. This is particularly the case if the patient needs regular insulin therapy in order to correct the chronic resistance to this peptide that can cause glucose toxicity. This form of treatment involves a consistent schedule of insulin injections. This form of medication may not be fun for many people with diabetes, especially as it often needs to be self-administered. This method can also reduce the motivation to stick to the treatment, which is in itself a serious issue for diabetic patients.
Why Diabetes Management Needs So Many Needles
Unfortunately, the few alternatives to regular self-injection are often not so fun for these individuals. They mostly consist of subcutaneous pumps attached to the body or clothing in order to deliver regular doses via a needle or cannula automatically.
Many patients may prefer to take their medication orally rather than any other route mentioned so far. But extraneous insulin cannot be taken by mouth. The supplementary peptides typically do not make it into the small intestine, never mind into the systemic circulation from this point in the gastric tract. They are attacked by stomach acids and dissolve away shortly after ingestion instead.
Furthermore, insulin has an incredibly short mechanism of action (or half-life) once it makes it into the system in any case. Therefore, biomolecules with this attribute are often only beneficial following injection. Nevertheless, many diabetic patients find the insertion of intravenous needles at regular intervals intolerable.
Therefore, a great deal of technical and engineering adaptation would need to go into a new alternative medication route for this condition.
Fortunately, a group of researchers from MIT felt themselves up to this challenge. This group, led by Giovanni Traverso of MIT and also the Division of Gastroenterology at Brigham and Women’s Hospital/Harvard Medical School, started off with the realization that an oral treatment regimen for diabetic patients would have to be one in which the insulin packaged into the new formulation was delivered directly to the small intestine.
To this end, they investigated the relatively new possibilities offered by the emerging technique of microneedle administration.
New Tiny Alternatives to IV Administration
Microneedles are typically made of stainless steel or some other medical-grade material. They are arranged on patches of an adhesive polymer, which are designed to be placed onto the skin so that the actual needles can pass through it and deliver a payload of a therapeutic compound. The microneedles are usually no more than a thousand micrometers in length, so as to avoid contact with sub-dermal nerves and thus avoid any pain from the patch’s application to the skin.
This new direction in bio-interface engineering may be a big part of the future of medical science and its translation into healthcare products.
However, the microneedles developed in the new MIT project could not be made out of metal. In fact, the team made their needles out of the insulin itself. These peptides in needle form, 'milli-posts,' were then arranged into a patch-like form.
The idea behind this creation was that the patch as a whole would spring out of a protective shell once in the small intestine, and then attach itself to the inside wall of this structure. As a result, insulin molecules would dissociate from the needles, en masse, and become distributed throughout the system via the small intestine’s normal mechanism.
Accordingly, the team developed a mini-capsule that was designed to open only when it reached the small intestine, which would be properly positioned to deploy the insulin-needle patch as it did so. This was done through the use of an outer shell material that could attach itself to the inner intestinal lining, yet also remain ‘upright’ at all times.
The process was achieved by giving the capsule a shape inspired by that of the leopard tortoise’s shell. This animal’s carapace has evolved in such a way that a tortoise, which has been knocked onto its back, can right itself automatically.

The capsule’s shape was based on the shell of the leopard tortoise (Stigmochelys pardalis), which allows the animal to passively re-orient itself. (Source: Bernard Dupont/Flickr)
This property, known as passive re-orientation, was thus conferred on the novel capsule so that the microneedle patch would always be capable of escaping and attaching itself to the appropriate tissue.
The team tested its new oral delivery system for insulin in experimental rats and pigs. In their new paper on the subject in the journal, Science, these preliminary animal trials have resulted in the behavior required of the capsule, and in appreciable systemic absorption comparable to a similar, transdermal microneedle arrangement.
Therefore, the team may have proven that oral treatment in diabetes management may indeed be possible, one day.
However, their new system may have a considerable amount of competition from the increasingly popular and well-studied option of transdermal devices incorporating microneedles. This technology is also accumulating interest from those in the diabetes research area. It may have the potential for greater treatment adherence compared to IV injections or subcutaneous pump infusions. In addition, recent studies have indicated that microneedle patches are getting better in terms of flexibility and confluence with challenging (e.g., wrinkled) areas of skin.
Therefore, this group from MIT may find themselves in a tight race towards next-generation diabetes therapies with these patches in the future.
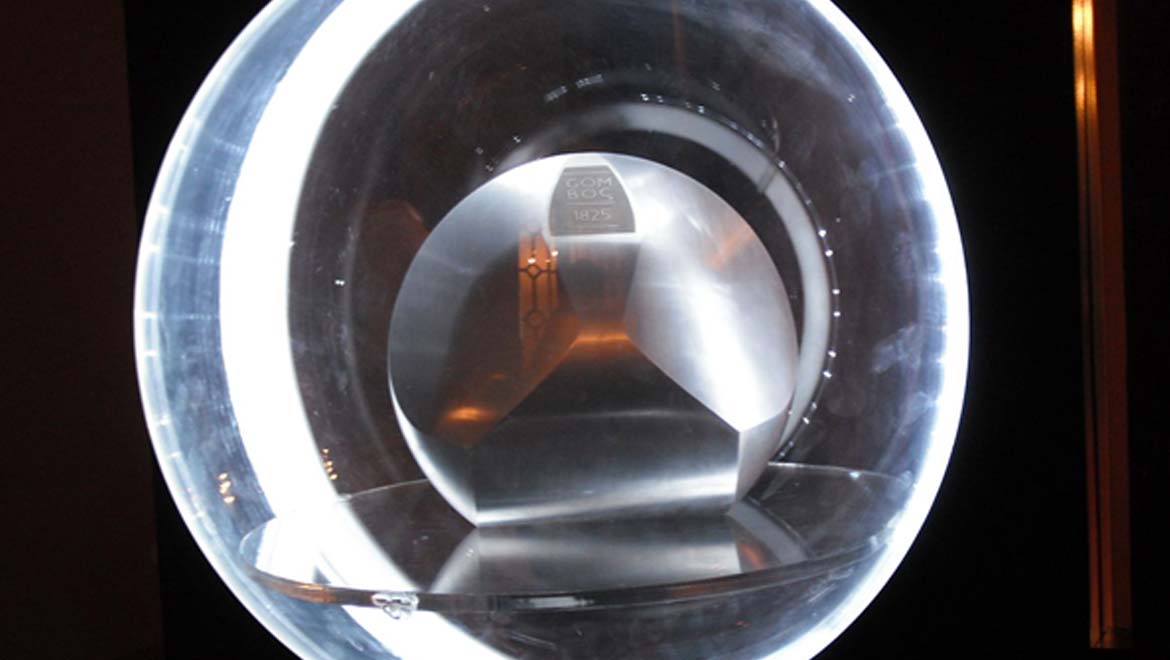
Top Image: A gömböc can also passively right itself as the capsule in the new oral insulin delivery system does. (Source: Gábor Hanák/Hanák Gábor (Cassandro)/Wikimedia Commons)
References
A. Abramson, et al. (2019), ‘An ingestible self-orienting system for oral delivery of macromolecules’, Science, 363 (6427), pp 611-615
Y. Zhang, et al. (2018), ‘Advances in transdermal insulin delivery’, Adv Drug Deliv Rev
A. L. Lewis, et al. (2015), ‘Challenges in the delivery of peptide drugs: an industry perspective’, Ther Deliv, 6 (2), pp. 149-163
M. Rajabi, et al. (2016), ‘Flexible and Stretchable Microneedle Patches with Integrated Rigid Stainless Steel Microneedles for Transdermal Biointerfacing’, PLOS ONE, 11 (12), pp. e0166330-e0166330






No comment